On the day of my pre-op consult, I had to be at the hospital at 8:30 am. We’d gotten a decent amount of snow the day before, so I took an Uber instead of the bus. I didn’t want to be late and didn’t want to risk delays because the streets weren’t plowed yet.
I had clear instructions — where to go and the order of appointments: bloodwork first, then an EKG and chest X-ray, and finally a meeting with my surgeon at 10:00. The friendly voice at the other end of the phone warned me to plan on spending the entire morning because things could run long. I packed my phone charger and water bottle, ready to work from the cancer center’s waiting room between appointments.
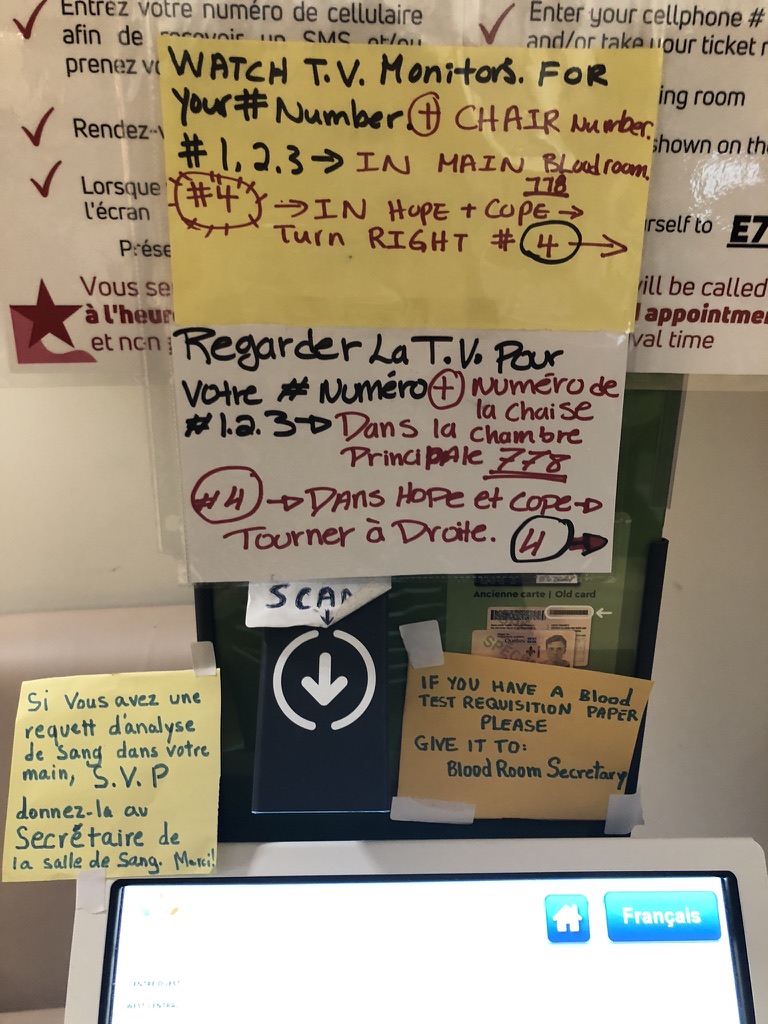
I should have known from the start that the day wasn’t going to go as expected. The self-checkin kiosk for bloodwork was a mess of bilingual Post-it notes explaining how to navigate the system. I felt for both the staff who had done this ‘fix it in the field’ hack and those who had to decode it as patients (me). Still, I persevered and the blood draw was uneventful. I liked the phlebotomist, who was deft with the needle.
Next up was the EKG, requiring me to navigate the corridors connecting different buildings. With years of wayfinding design in my work history, this shouldn’t have been hard, but hospitals are a special case of signage systems that have been bolted together. Eventually, an orderly guessed I was wondering if I was going the right way and invited me to follow him. A short wait later, the EKG took less than 10 minutes to complete.
Now familiar with the hospital’s signage intricacies, I found Radiology without a staff member to guide me. It was going on 9:30 at this point and it crossed my mind that my 10:00 appointment with my surgeon was at risk. I shouldn’t have been concerned.
X-ray complete, I navigated back to the Gynecologic Oncology floor feeling like I knew my way around. As I got off the elevator, I heard a staff member calling my name and thought the timing was perfect. After filling in more patient information, and checking my weight and height one more time, she pointed to the waiting section and said, ‘have a seat, we’ll call you.’ It was now going on 10:30.
I settled in and pulled out my phone, prepared to triage my inbox for work. Not that far into the exercise, my phone battery was at less 20%. Digging into my bag, I pulled out an iPhone cable and my battery pack. I fiddled with the cable in a way that all iPhone users understand, and then watched in dismay as it gave up the ghost with a puff of smoke where the cable met the pronged end you’d insert in your phone. I conserved the rest of my battery to let my best friend know how to find me — she was on her way to meet me and offer moral support.
The next few hours passed watching patients come and go while we waited … and waited … and waited some more. Eventually, my friend had to leave to get back to her work day and I was left to eye the cookies and juice as a poor replacement for lunch. Paying attention to the conversations between staff, I could discern there were rounds underway, and that was followed by an all-hands tumor board meeting. No one said anything, but I resigned myself to it being a long day. It was 2:30 before my name was next up.
I had come prepared with a list of questions along with copies of my biopsy pathology and ultrasound report. But of course, they were on my phone and not paper copies. Lesson learned. Always bring an analog backup. The resident with my file seemed surprised I could play back the pathology without the digital version. Still, I liked her immediately when she lent me her phone cable so I could recharge my phone while we talked. Eventually, she found my report files in the system that – in theory – provides an integrated patient profile. After what seemed like repeating answers to the same patient profile questions for a third time, she did a brief pelvic exam and then reviewed the surgery plan in detail, answering my questions as we went.
A complete hysterectomy, bilateral salpingo-oophorectomy, and sentinel lymph node dissection. Performed robotically. If all went according to plan, I’d be home in my bed at the end of the day. No need for an overnight stay. I was pleased we could confirm that it would be robotic. I had been concerned that fibroids might make that approach difficult.
The surprise was that my doctor wouldn’t necessarily be the one doing the procedure on the day. I learned the gynecologic oncology surgeons work as a team, so any one of them might be lead when my procedure was scheduled. I didn’t love that answer, but didn’t hate it either. It meant more research on my part to learn about the other team members.
Pre-op includes signing any number of consent forms. Mine included the option of banking my pathology for clinical trials. While I didn’t know the rest of my surgical team yet, I did know one of them contributes to a trial that aims to develop a screening test for endometrial and ovarian cancer. That project has a local 5K race to raise funds. I’m not that superstitious, but I took it as a good omen.
Forms signed, paperwork sorted, all that remained to discuss was timing. My gynecologist had said to expect surgery within 30 days of my consult, so I was surprised when the answer was eight weeks, maybe six.
Despite this longer wait for surgery to be scheduled, one bright piece of news was returning to running after my three-week post-op follow-up was discussed as a possibility, all dependent on recovery progress and pathology results.
By 3:30, I was on my way home, processing this new timeline for surgery, the reality of more waiting, and preparing to update my friends and family.
Leave a comment