Similar to any good training plan, my chemo treatment plan has weeks that offload the strain on my body, intended to allow for healing and recovery, and to minimize the cumulative toxic effects of the drug regimen. Mostly that has been working well for me. Still, just like when you are two thirds through a build, where I find myself now is understanding the remaining weeks of treatment will be a grind. We all go through it.
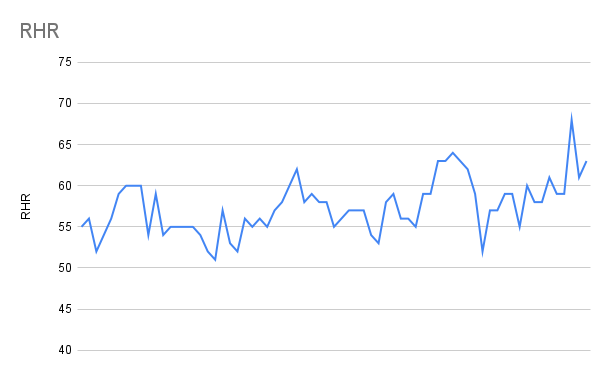
I have enough data from the last twelve weeks to see the patterns that create this situation. My resting heart rate is higher, my weight has a repeating fluctuation, I need more sleep to feel rested, and despite wanting it to be a different curve, a workout takes more out of me than it did in the beginning. All of these are reasons to persist, but it is challenging when the metrics show you that it’s harder on your body.
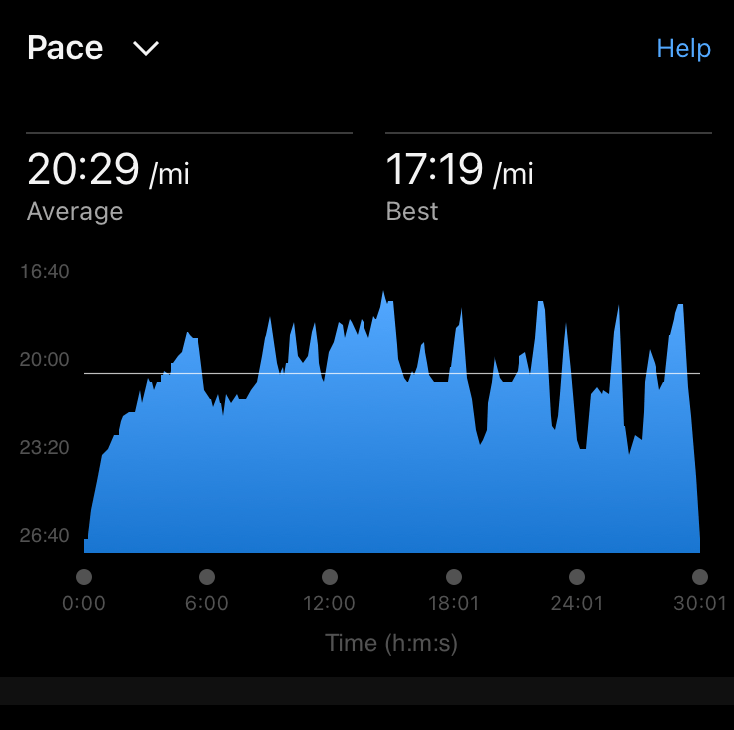
One way I’m tackling the issue is looking for different metrics than pace and perceived effort as motivation.
Impact on side effects
I’ve been reasonably lucky so far that aside from an elevated resting heart rate, my side effects have been limited to bone and joint pain for a few days that is mostly managed by minimal pain medications. This past cycle, however, I’ve noticed neuropathy creeping into my right hand, even though I ice both my hands and feet during treatment. The good news is there is evidence that exercise during chemotherapy, especially taxane-based treatments like mine, show an improvement in neuropathy and quality of life.
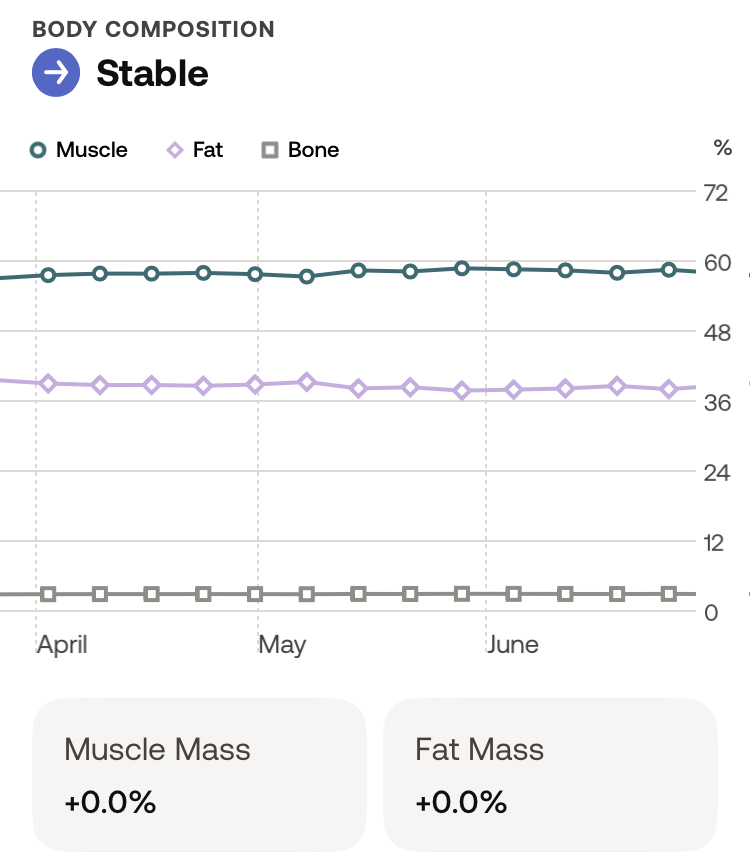
Another concern during chemotherapy is loss of strength and muscle mass. My data shows me that my body composition has remained stable since I started treatment, and both my oncologist and I attribute that to consistency. My paces may be slower, and my time on feet shorter these days, but it is enough to keep my base in place.
My hurdle to navigate over these last two cycles is the cumulative impact of treatment on my bloodcounts — both neutrophils and platelets — a known side effect that is a dose-dependent situation, ie: it can get progressively worse with the number of treatments. For the last two cycles, my counts have been lower than ideal, to the point that we discussed additional medication should they not recover in time for the next infusion. Fortunately, I’ve avoided that so far. I say fortunately because what comes with those medications is more bone pain.
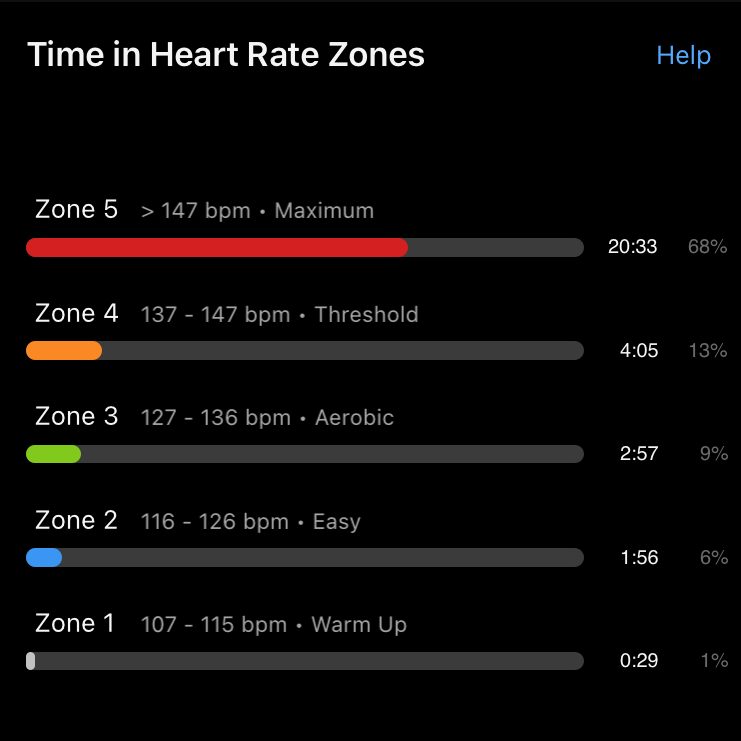
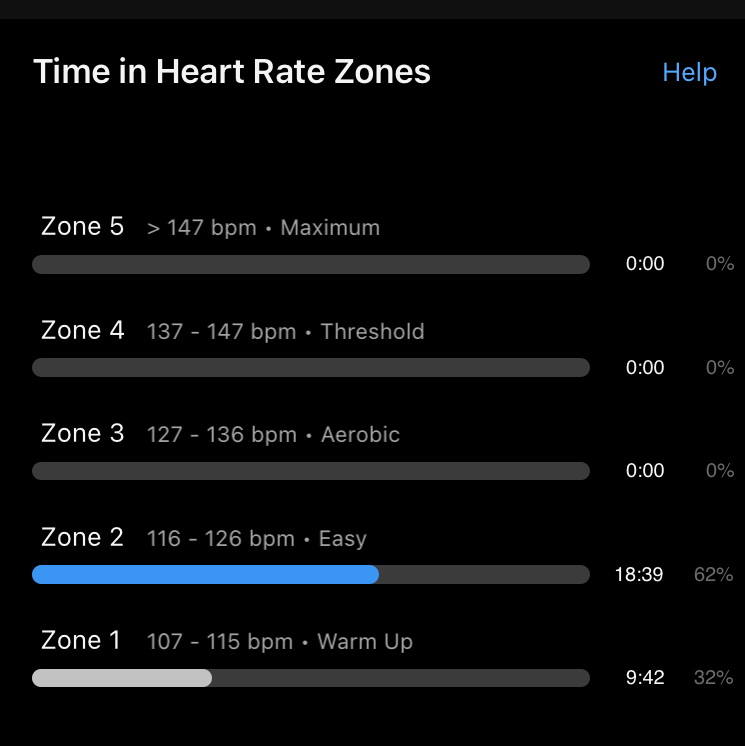
What it does mean is that I notice my endurance is lower because of low platelets, and I have to be conscious of what I eat and where I go because of low neutrophils. It’s all a balancing act to manage energy levels and risk of infection. The same workout that is normally a Zone 2 effort can feel like Zone 5 in these situations, and I invoke spoon theory — is the number of spoons I’ll use to complete a hard workout worth the time I know it will take to recover on the other side? The answer is different on different days and I remind myself that rest is an active choice.
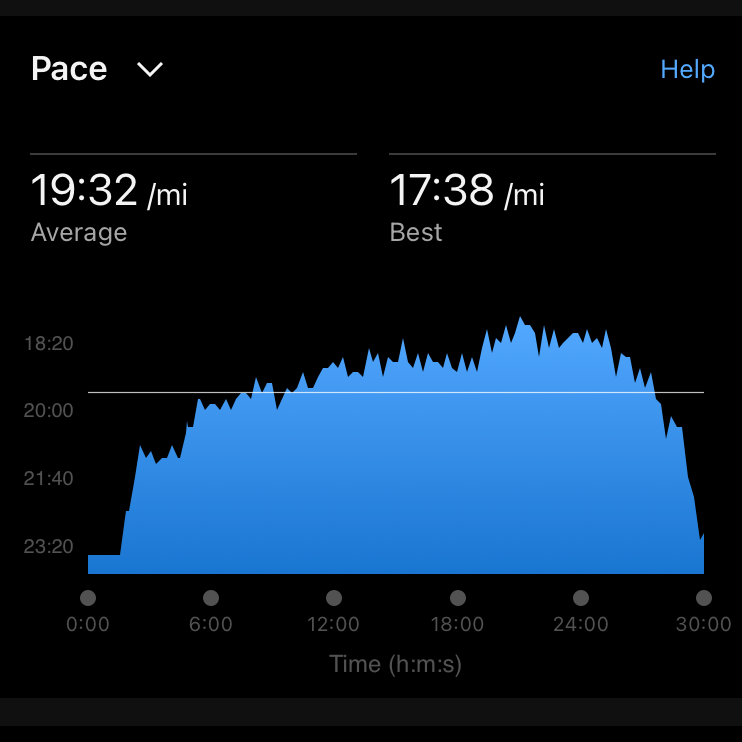
The same workout, two days apart, can feel very different
A bright spot is that I’ve discovered dark chocolate increases your neutrophils, so who am I to deny science?
Keeping an eye on the finish line
I’m at that point in my treatment plan where things are getting harder — not so much physically but my mental game takes more effort to stay focussed on the goal. It’s not unlike the back half of a race, where even if you’ve not gone out too fast (my worst bad habit), you start to feel how much work its going to take to get to the finish line. We all know the grind is part of the process.
I am still in the race, and still focussed on the finish line. It’s just that I appreciate the grind it will take to get to that reward.
Leave a comment