It’s been four weeks since I wrapped my EBRT sessions—and my flu and Covid vaccine boosters were two Fridays ago. The flu shot was the thing that made me pause—because I’m no longer on active treatment. Yesterday, I saw my radiation oncologist for my first follow-up visit and I won’t see them again for six months. A whole new chapter is beginning to unfold—survivorship.
Cancer is not what you think it is
Cancer is not what you think it is. Or at least it hasn’t been for me. Yes, I remember that moment walking into the operating room where it felt like I was in my own episode of Grey’s Anatomy, but with the exception of dealing with my early symptoms, and those first few days of post-surgery recovery, I’ve never thought of myself as ‘sick.’
Though I’ve had a wig that served me well during Zoom calls with work colleagues, by and large I’ve gone most of this past year ‘topless,’ choosing instead to rely on hats when I needed to protect my fuzzy head and not make others around me uncomfortable. And now that my hair is coming back, I have a lighthearted Thread about the experience—The Hair Chronicles—both because I’m fascinated, and because you have to look hard to find references online.

I’ve managed this last year with some very specific constraints—no lifting anything over 10 lbs post surgery, protocols to protect my compromised immune system during chemo, and a whole new level of hydration during radiotherapy—but by and large my life has been about what I could/can still do as I moved through active treatment. To the surprise of my team, and to me, that’s included more running than I expected.
Still, I wasn’t prepared for the feeling of being totally unmoored on my first Friday with no scheduled treatment. With my radiation oncologist follow up appointment a month out on the horizon, I found myself completely distracted and focus was a challenge. In the end, I emailed my clients and let them know I was taking the day to allow my brain to catch up with my body’s reality of getting on with finding an equilibrium that didn’t include chemotherapy or radiation. Three weeks on, I think it’s slowly sinking in. And I’m finding smaller changes that show me I am healing, not from the disease, but from the treatment.
Rewriting a training block
The interesting thing about this timing is that is falls on my calendar in a very similar pattern to fall racing. November is when I would have fall races behind me and I typically would take the month, and maybe even most of December too, to treat running lightly and regroup for a spring racing plan. So this feeling of ‘maybe I’ll run, maybe I’ll stream something instead,’ is familiar.
In fact, I haven’t run in the last week, while I try to isolate whether my on again/off again sore right hip is running-related or an artefact of treatment. The resident I chatted with yesterday (also a runner) agreed with my isolation of it likely being an SI joint alignment issue, and told me to keep an eye on it as I rebuild my mileage. Not surprisingly, your bones near the SI joint are vulnerable to injury after pelvic radiation because of their location in the treatment field.
I haven’t yet sat down to update a training block, but I am deep into looking at 2025 race calendars to pick my choices. Right now, I’m leaning towards 10ks in the spring, and a half or full in the fall (I know, I know). And though I enjoy travelling for races, I’m feeling more like I want to lace up my shoes locally. Fortunately, Montréal has a wealth of options. And I have running friends who’ve volunteered to come to me so we can race together.
Training post-treatment
When I was first diagnosed, one of the things I discovered was that endometrial cancer survivors have an elevated risk for cardiovascular disease— as much as 1.5x the average population. The working theory is this is tied to body weight, with many patients being obese. More interesting to me is research looking at how low muscle mass can co-exist with excess weight and that it may impact cancer treatment and post-treatment survivorship.
Dr. Carla Prado is a researcher at the University of Alberta and a member of the Women and Children’s Health Research Institute. She has studied how cancer patients can have excess body fat and low muscle mass at the same time, and how cancer treatment can make low muscle mass worse. I’m not the biggest fan of solving through yet another digital tracking program, but I do like that her current research acknowledges, ‘endometrial cancer survivors, in particular, have been underrepresented in research on nutrition and physical activity.’
Body composition changes over time and women lose between 3–5% of muscle mass per decade as we age. Taken in context with the increased risks that come with being an endometrial cancer survivor, strength training rises even higher on my training priorities.
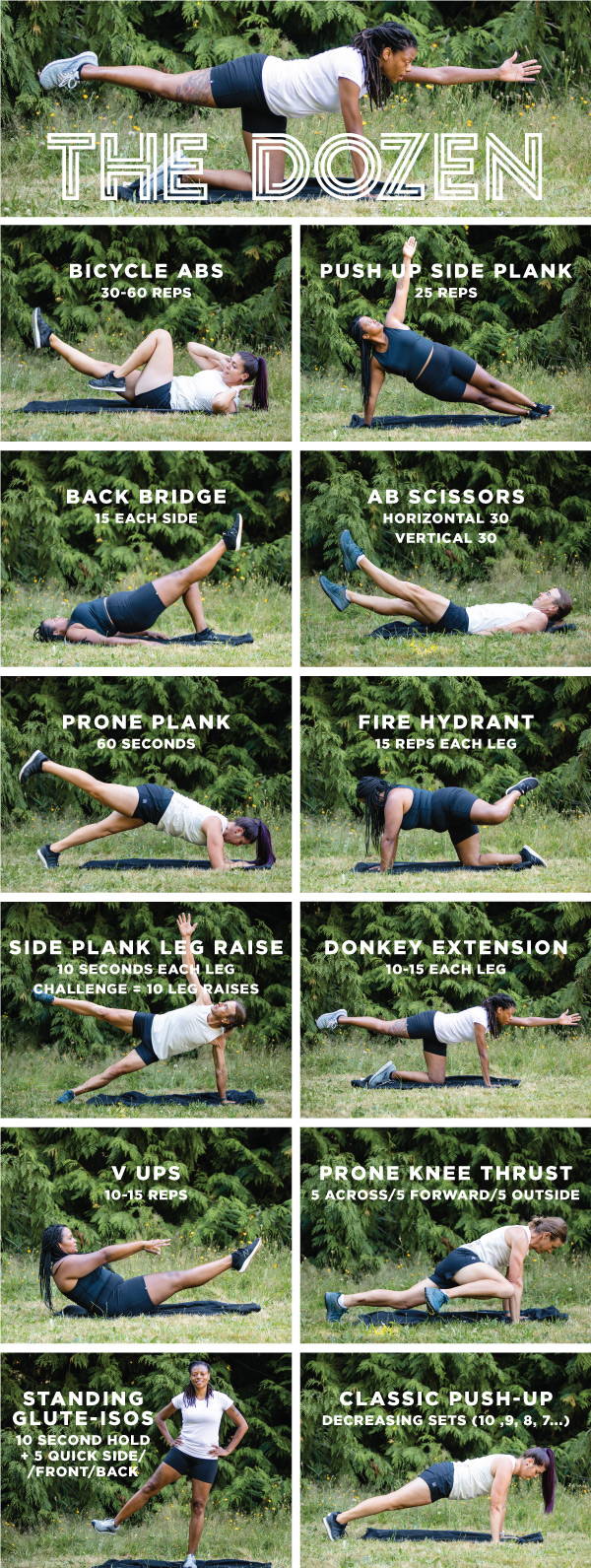
Like a lot of runners, I’m notoriously bad at including strength training. But fortunately, my running team has resources that I’m incorporating in this new phase. ‘The Dozen,’ is a great set of core exercises, and I’m exploring Lesko’s 4 week strength routine because we share a similar age, though she is a far more committed runner than I am.
Base building from the ground up
Both my pace and time on feet ebbed and waned during treatment. Right now, I’m not that fussed about pace, but I do want to rebuild my base into a solid 15+ miles/week. That means 3 shorter runs of 2-3 miles, one tempo work out and one long run each week. I’ll still pay attention to my body, but I’m ready to push the envelope and discover where my endurance can take me at the moment. The last few times I’ve run, I’ve been able to pick up my pace but still feel like there’s something left in the tank, and I’m taking that as a good sign my body will respond well to increased mileage.
Forward is a pace
Looking ahead, I find myself wondering how treatment has impacted my overall ability to train.
At yesterday’s appointment, we talked about how there is so little reference for what survivorship looks like for women, and especially so for active athletes at all abilities and ages. Before I started radiation, I talked with my oncologist about pelvic and hip fractures because of the impact on bone density. He counselled that running was not a real risk, but falls—or hard, sudden impact—would be, so I’m not likely to tackle any technical trails in the near future. Yesterday though, when I mentioned I was updating my blog, the resident who was processing my updates was interested and told me how underserved she felt both patients and doctors were because of the lack of research—and even first hand stories—available.
In a lot of ways, this feels like 10+ years ago when I started running seriously again. I know what my body could do once, and I have muscle memory that makes training feel familiar, but the road ahead feels like a brand new route that is likely to yield surprises along the way.
More as I discover what those might be.
Leave a comment