I’ve read that your body uses as much energy through surgery as it does during a marathon. True or not, that’s been a useful benchmark for the last couple of days since I was discharged Thursday evening.
A chat with my surgeon pre-surgery reset what recovery might look like, and she has been right. When I shared a running friend’s description that post-hysterectomy felt like having trashed your legs after a race, but someone also dropped a bowling ball on your stomach, her immediate response was ‘oh, that wouldn’t have been a robotic procedure then.’ We talked sore hamstrings being a reasonable expectation after four hours of surgery, given the stable position required, but she emphasized the bigger risk would be not doing too much.
The race: Surgery
My surgery was first on Thursday’s schedule. I arrived at 6:30am and navigated peri-operative paperwork and bloodwork before being taken up at 8:45. I was introduced to the whole team as I was walked into the OR. It felt as if I was in my own episode of Grey’s Anatomy. Beyond a fun chat with my anesthesiologist and her assistant as they placed my IVs, my next memory is waking up in the PACU about six hours later.
A nurse gauged my pain level and a dose of Dilaudid was delivered via my IV. After a huddle about my respiration, pulse and blood pressure being lower than expected (enough to set off alarms from my monitors), the PACU team decided I was doing fine and moved me to a room on the fifth floor to be monitored until I could walk, eat solid food, and ‘process liquids.’
In my room, I had low-flow oxygen until my sats stabilized and my respiration came up to a more ‘normal’ level — I could see my nurse visibly relax as it settled into what she felt was OK. I didn’t have the energy to explain to her that as a runner, my resting heart rate was somewhere in the low 50s, and dipped into the 40s on a regular basis. And that’s compounded by blood pressure that charts low on a normal day.
When my surgeon arrived with the good news that I could sleep in my own bed that night, she backed me up that my readings were where she expected them to be. Surgery had gone to script, a little longer than planned but with no big surprises. We reviewed the details and she left with a caution to stay on top of any pain for the first 48 hours, and not to overdo it until she saw me in 3-4 weeks to discuss my pathology results and plan any further treatment that might be recommended based on that.


One hospital dinner later, it took two IVs of fluids and another two pitchers of ice water for my bladder to wake up and realize it was the last item on the checklist before my best friend could pick me up. By 9:30pm we were on our way to my apartment.
Home, my BFF was surprised by how chipper and alert I was. A friend on the west coast reminded me that anesthesia includes a dose of adrenaline. I was still in the throws of an adrenaline rush that wouldn’t wear off for hours yet.
Post Op Day 1: Friday
For the first time ever, even though I was in bed for eight hours, and I would swear that I slept for most of that, my Garmin read ‘no sleep data’ when I checked my watch Friday morning.
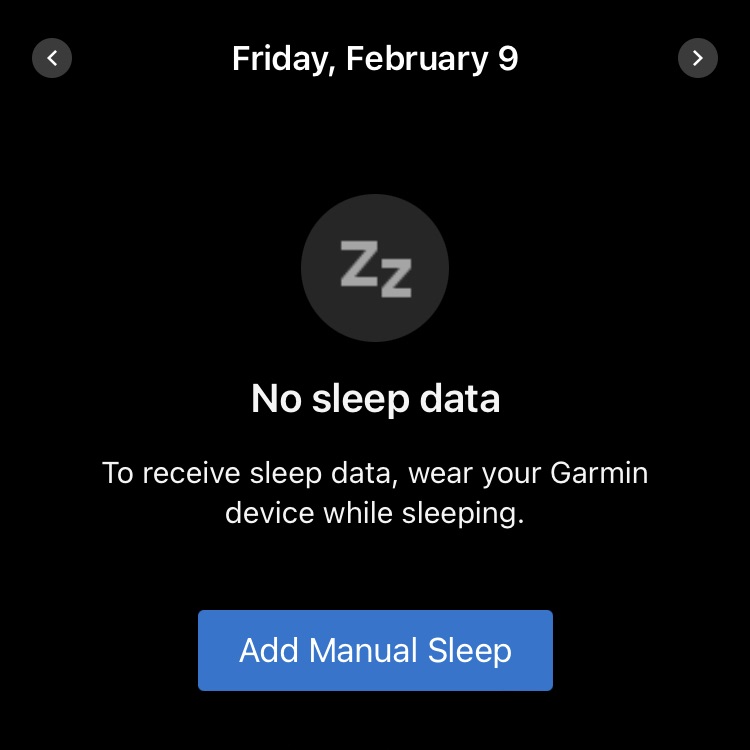
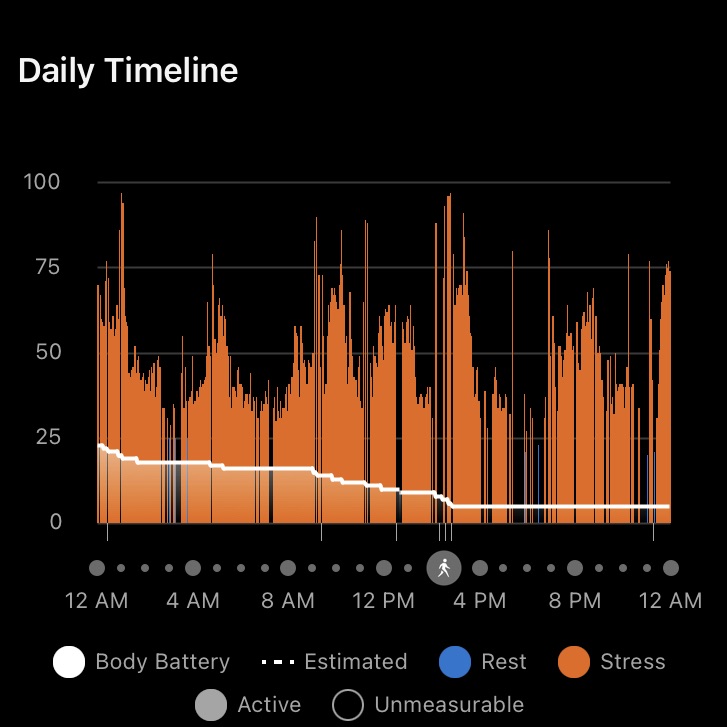
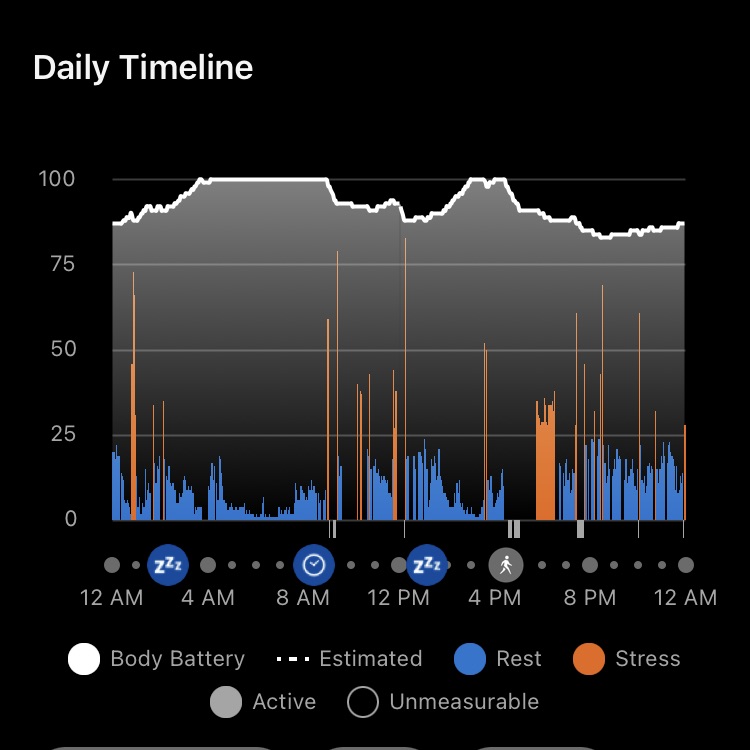
I woke up starving — a clue that my body was doing double time even though I wasn’t exerting any energy. My Body Battery had only inched up to 23 from 5. As the day wore on, it slid down to 5 again, while my stress levels stayed in the ‘high’ register — this despite me spending most of my time lounging in my chair and a half while my BFF fussed over me, cooking and making sure I stayed well-hydrated.
In the afternoon, we took a short walk around the lobby of my building before another friend dropped by to visit after his run and the three of us had an early dinner together. Whether the adrenaline was still from the anesthesia, or just naturally produced, it was midnight before I was ready to sleep again.
My pain level throughout the day was minimal. I described it to my friends, and my siblings when I spoke with them, as having sore abs from a core workout versus how I had expected to feel post-surgery. I managed it with Aleve and Tylenol on an alternating schedule.
Post Op Day 2: Saturday
It’s amazing the difference a good night’s sleep will make. Friday night I didn’t set an alarm to take pain medication and slept through until Saturday morning. I woke up hungry — again — but went back to sleep until almost 10am, when my Recovery@Home nurse called to check in on me. That call was followed by a second one from my doctor, with the good news that my ultrasound mammogram results were already available — and everything was clear!
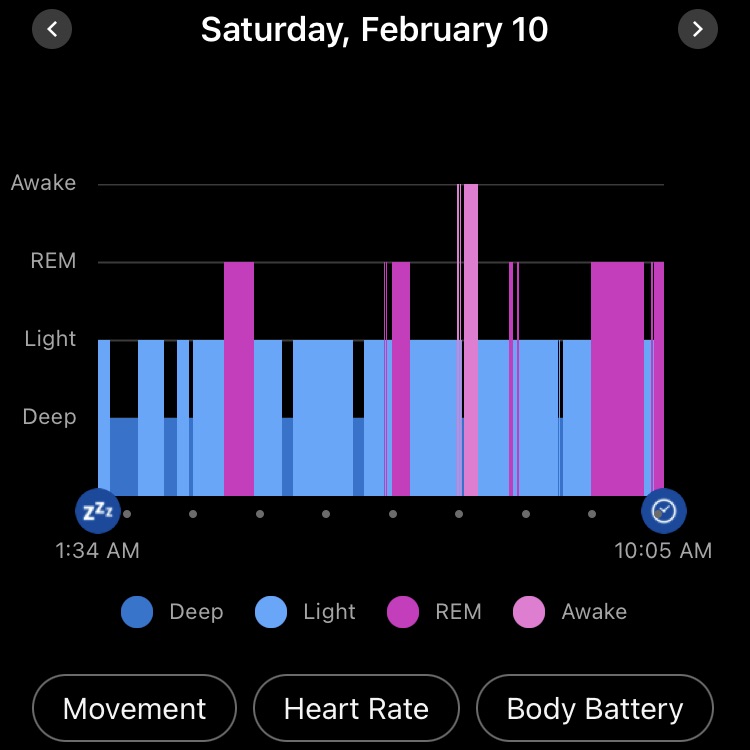
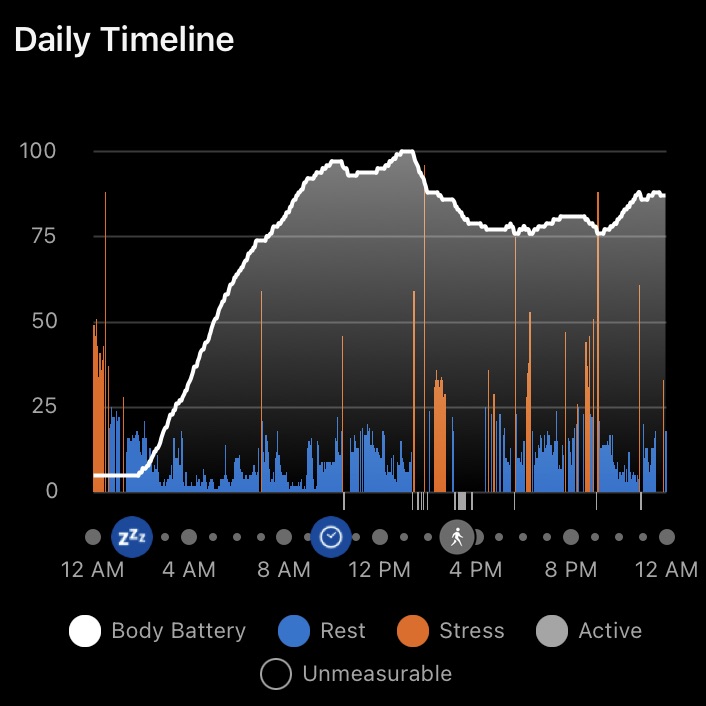
Saturday afternoon my BFF and I ventured outdoors and we walked 1.5 km in spring-like temperatures. I was surprised at how good I felt and probably could have gone further.
We spent the rest of the day running lines — my BFF is an actor and she had an audition coming up — before I sent her home at dinner time, confident I could manage on my own but with a promise to check in if I needed anything. I settled in to watch West Wing reruns before I called it a day around midnight.
Post-op Day 3: Sunday
Even though Saturday was a marked improvement over Friday, it was waking up today — Sunday — when I realized I finally felt like myself. I stretched in bed before I got up, doing some deep breathing exercises to engage my core and make sure my lungs were clear. My resting heart rate was back down in the mid-50s and my stress level looked like a typical daily graph. We’re only at the beginning of this healing journey, but my body felt like it had figured out the last few days, gotten over the shock, and was now ready to get on with the business of mending itself.
My Recovery@Home nurse officially discharged me after our morning call, and I made myself a riff on a vanilla latté — french pressed beans frothed with a scoop of vanilla-flavored protein powder. Then I bottled the Greek yogurt I had left to strain before I went to bed so I could make my favorite breakfast bowl — yogurt, sliced banana, mixed field berries, and a scoop of low carb muesli, topped with maple syrup.
Wound healing is a catabolic state — so carbs and protein in plentiful supply are key. I’m still investigating what that means for dialing in my diet — which centers whole foods, and a lot of cooking from scratch. One change is adding snacks when my body gives me hunger cues — today that was a pear and Brie before I went for another 1.5 km walk around the neighbourhood, and some stoneground crackers and guacamole this evening while I wrote this post. Dinner was beef stir fry with onions, mushrooms, yellow pepper and zucchini.

All in all, after my first day solo, I’m winding down, a little tired, but pain-free and well-fed. 5,000 steps feel like a good baseline for the rest of this first week, and my energy level has stayed strong throughout the day.
What’s next?
Treating the lead up to my surgery as a training block has paid dividends. The things I worried about in the immediate post-op transition have not transpired for me — my experience with gas pain from insufflation as part of surgery was limited to being a little uncomfortable the first 24 hours but resolved by the second day; the fatigue that some of my friends described hasn’t been a factor so far; I haven’t had problems with leg and ankle swelling as a result of lymph node removal; and now I understand why my surgeon repeated that I should make sure not to push it too far too fast, because other than taking two Aleve this morning, I haven’t been conscious of pain as I moved around today, doing day-to-day things like cooking, washing up, and going for a walk.
I have to wait 3-4 weeks before the pathology results from my surgery will tell us whether there’s any further treatment required. Until then, I’ll be taking it easy this week, slowly easing back into work — which is part-time and remote, and walking different routes in my neighbourhood, trying not to be jealous of the runners I pass.
Leave a comment